1. The environment is the most significant contributing factor.
- The environment is most definitely a contributing factor and obviously the colder weather and the longer the exposure the greater the chance of a drop in core temperature, however the most common cause of a drop in core temperature in TRAUMA is blood loss.
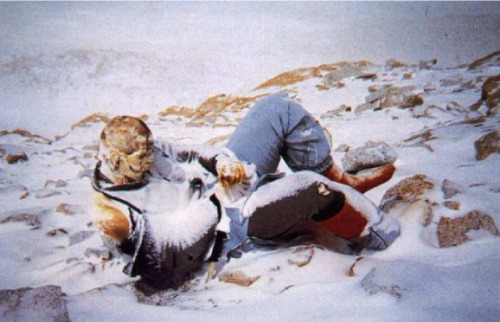
- When we think of hypothermia patients we often visualize someone summiting Everest, or submerged in cold water, or a Boy Scout lost in the woods for days on end. Hypothermia cases like those are the ones we learn about and discuss when we are taking EMT class, first aid course, or in wilderness medicine classes. In these cases Hypothermia is often the primary injury, perhaps accompanied by frostbite. This type of Hypothermia is primarily due to exposure, it may be a result of a fall or accident but prolonged exposure is the primary cause of the loss in core temperature. Hypothermia in Trauma is a very different animal.
- Normal core temperature is 98.6 F / 36 C at that temperature the body is in Homeostasis essentially it’s “Happy place”. The body has no heat pump, heat is the byproduct of metabolism. Aerobic metabolism relies on oxygen being delivered to the cells by red blood cells (RBC’S). When trauma patients bleed (and they often do), they lose RBC’s thus reducing the amount of oxygen that's delivered to cells. This poor perfusion(shock) results in a reduced rate of heat production and a drop in core temperature. This drop occurs with or without environmental factors.
- The first step in preventing hypothermia in a trauma patient is also the first step in our M-A-R-C-H mnemonic, Major Hemorrhage - Stop the bleeding as quickly as possible and preserving every drop of blood. Hypothermia is important and gets it’s own letter in the mnemonic (marcH). You begin to preventHypothermia the second you initiate hemorrhage control measures.
2. Hypothermia is uncommon and not lethal.
- 66% of Trauma patients become hypothermic and almost all patients suffer a drop in core temperature.
- Mortality was twice as high (53%) in patients with a Core Body Temperature<32°C compared with patients with a Core Body Temperature<34°C (28%)
- Shock is a common finding in trauma patients and often a good clinical indicator that a patient is close to death. Shock is defined an inadequate perfusion, again oxygen not reaching the cells.
- The Trauma triad Hypothermia - Coagulopathy - Acidosis is a vicious circle when one portion occurs it exacerbates the others. It’s a cycle we as providers must be aware of and aggressively disrupt to increase a patients survivability.
3. A blanket is the best treatment for hypothermia.
Image source: Emergency Zone
- As we already stated the best treatment is prevention, if your patient is already hypothermic it’s almost too late. Focus needs to be on prevention and not treatment.
- Wrapping up a casualty in a blanket or a mylar blanket (passive re-warming) are all based on the principle of trapping or reflecting the patients heat. Trauma patients that have lost blood externally or internally are in an aerobic metabolic state and lose their ability to create their own heat. You must actively rewarm the patient, utilizing some external heat source, heat packs, warm water bottles, bear hugger, HPMK, blizzard blankets, etc….) a blanket by itself will not do the job well even with a naked Ranger buddy / swim partner.
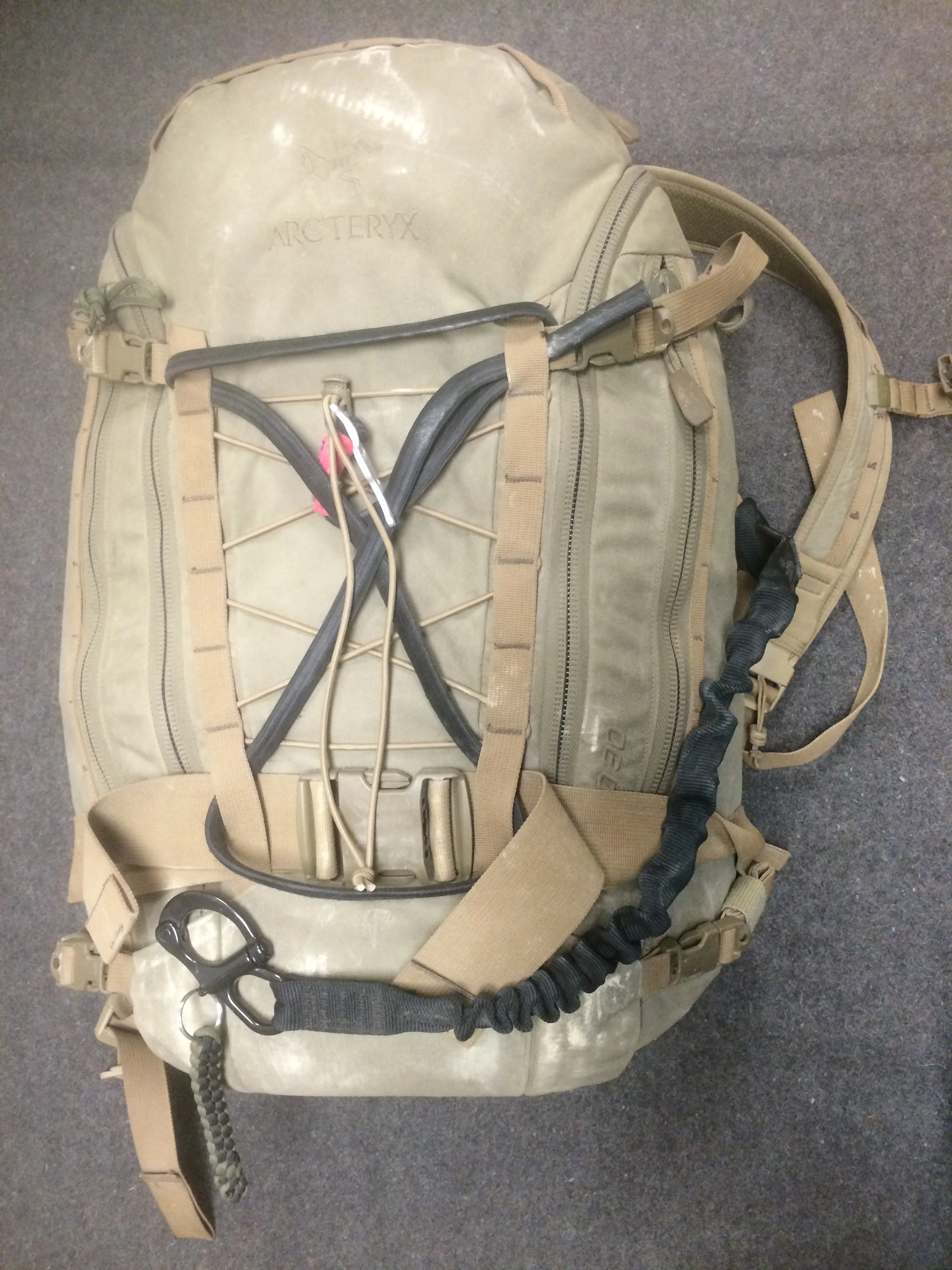
NAR HYPOTHERMIA PREVENTION AND MANAGEMENT KIT (HPMK) courtesy of North American Rescue
- We’re not saying not to utilize a blanket, just understand that a blanket alone will take a very long time to increase core temperature and covering a casualty limits your ability to monitor patient (check tourniquets, monitor bleeds).
4. Hypothermia is not a FIRST-responders concern it’s the Trauma centers PROBLEM
- It can be easy to have this mentality when the first people to treat casualties are only working from an IFAK (Individual First Aid Kit), which has nothing to take or monitor temperatures and very little if anything to treat a hypothermic patient.
- Hypothermia prevention and treatment was not something we as military medics focused on in 115 degree weather in Iraq early on in Operation Iraqi Freedom (OIF), when Tactical Combat Casualty Care (TCCC) was a new concept to many of us. The Pre-Hospital Life Support (PHTLS) standard of care was 2 large bore IV boluses, running cold salt water into a trauma patient and then transporting them at altitude in a helicopter for prolonged periods of time. Not so coincidentally when we changed our approach ( IV fluid only when hemodynamically unstable) and put an emphasis on hypothermia prevention & treatment our military casualty fatality rate (CFR) decreased.
5. Shivering helps and will indicate my patient is cold.
- Shivering is a muscular contraction that indicates a drop in core temperature and early onset of hypothermia.
- Shivering just like any other muscle activity increases the demand for oxygen. When we exercise the increase in activity creates an increase in oxygen demand. Shivering is a muscular activity and a casualty that’s shivering will have a 400% higher demand for oxygen and an increase in intercranial pressure.*6 That's a bad thing for someone that's already perfusing poorly.
- Shivering is most likely to occur when the core temperature is 34-36°C,*7 diminishing with core temperatures below 34°C.The ideal goal in shivering management is prevention. Every effort should be made to avoid shivering stimuli and to stop shivering
activity when it starts.*8 The strongest evidence in the literature related to the cause and prevention of shivering supports protection of cold-sensitive cutaneous receptors from direct cold contact.*9 Avoiding skin exposure and contact with cold surfaces
should be the first step to minimize the risk of shivering in patients undergoing therapeutic hypothermia. Other non-pharmacological treatment of shivering is the application of warm packs to the face and arms.*10
"An ounce of prevention is worth a pound of cure"
Benjamin Franklin
Related Articles:
Trauma’s Lethal Triad of Hypothermia, Acidosis & Coagulopathy Create a Deadly Cycle for Trauma Patients
Hypothermia in trauma: The cold, hard facts
References
- Helm M, Lamp L, Hauke J, Bock KH. Accidental hypothermia in trauma patients. is it relevant to preclinical emergency treatment? Anesthetist, 1995 Feb;44(2):101-7.
- Hypothermia in trauma: The cold, hard facts DARIA C. RUFFOLO, RN, MSN-CS, CCRN, ACNP
- Frisch, D. E. (1995). Hypothermia in the trauma patient. AACN Clin Issues, 6(2), 196. 27.
- Jurkovich, G. L., Greiser, W. B., et al. (1987). Hypothermia in trauma victims: An ominous predictor of survival. J Trauma, 27(9), 1019.
- Tsuei BJ, Kearney PA. Hypothermia in trauma patients. Injury 2004;35:7-15.
- Rosa G, Pinto G, et al: Control of posy anesthetic shivering with nefopa, hydrochloride in mildly hypothermic patients after neurosurgery. Acta Anesthesiol Scand 1995; 39:90-5
- Lopez M, Sessler DI, et al: Rate and gender dependence of the sweating, vasoconstriction, and shivering thresholds in humans. Anesthesiology 1994;80:780-788.
- Flacke JW, Flacke WE. Inadvertent hypothermia: frequent, insidious, and often seriours. Semin Anesth 1983;2:183-196
- Sato H. Fusimotor modulation by spinal and skin temperature changes and its significance in cold shivering. Exp Neurol.1981;74(1):21-32
- Benson L. Shivering in patients recovering from CABG. Crit Care Nurse. 1998;18(5):92-93



















5 Essentials items for an IFAK, Bug out bag or first aid kit.